What is shoulder arthritis?
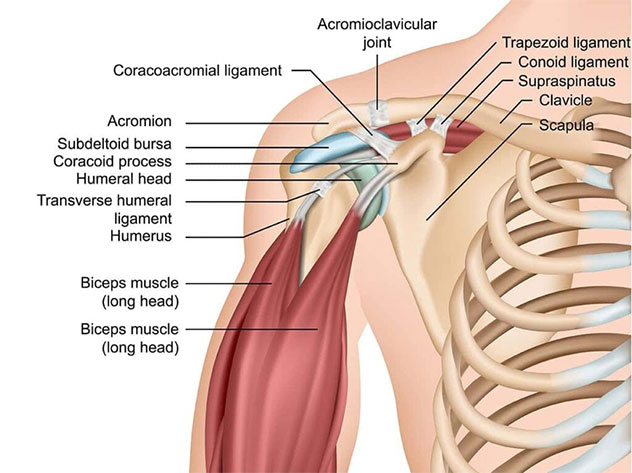
The shoulder joint is made up three bones – the humerus (armbone), scapula (shoulder blade), and the clavicle (collarbone). The ball and socket component of the shoulder is termed the “glenohumeral joint”. This refers to where the ball part of the humerus moves on the socket part of the scapula. The joint surfaces are coated in an extremely smooth cartilage lining which helps lubricate the joint and allowed for frictionless motion. The shoulder is after all the most mobile joint in the body!
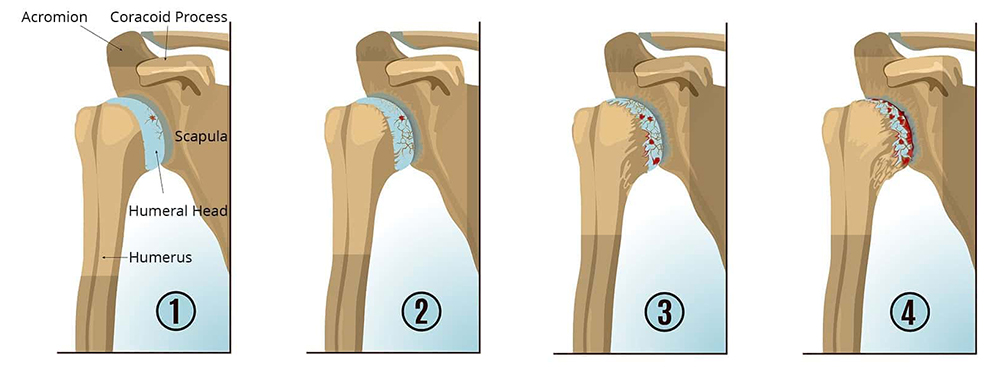
For many possible reasons, the cartilage coating the joint surface of the bones can become damaged and worn out. When this occurs, the body is unable to replace it with the same type of smooth joint cartilage. Eventually, what was once joint cartilage becomes irreversible exposed bare bone. When this occurs on both sides of the joint, it is sometimes referred to as “bone-on-bone” arthritis
How is shoulder arthritis caused?
Arthritis has many possible causes, including:
- Osteoarthritis – a degenerative condition leading to damage of the joint cartilage of the shoulder. Also referred to as “wear-and-tear” of a joint.
- Rheumatoid arthritis – an autoimmune condition which leads to inflammation of the lining (synovium) of the joint, which eventually leads to destruction of the joint cartilage.
- Post traumatic arthritis – damage to the joint cartilage as a result of a fracture involving the joint surface, or due to recurrent dislocations.
- Rotator cuff arthropathy – as a result of long-standing damage to the rotator cuff tendons supporting the shoulder, altered biomechanics leads to eventual joint surface disease.
- Avascular necrosis – loss of blood supply to the bone of the humeral head leads to collapse and destruction of the joint.
- Fracture – a bad broken bone involving the upper part of the humerus may not be reconstructable and joint replacement may be a more reliable solution.
The most common causes of shoulder arthritis are osteoarthritis and rheumatoid arthritis. These primarily affect patients over the age of 50.
What are the symptoms of shoulder arthritis?
Shoulder arthritis can be very debilitating, particularly in the advanced stages. Some of the symptoms include:
- Pain around the shoulder, usually a dull ache, and worse when attempting to move the arm. Pain can radiate from the shoulder to the neck or down the arm.
- Crunching and clicking inside the shoulder, particularly when trying to move the arm.
- Stiffness and loss of range of motion – particularly when trying to rotate the arm or lift the arm above your head.
- Swelling around the shoulder – this is the result of joint fluid accumulating within the arthritic joint.
- Loss of function – in particular when trying to reach your hand to your head and face, or when trying to get dressed.
These symptoms become worse and more pronounced when arthritis progresses.
How is shoulder arthritis diagnosed?

In addition to a careful clinical examination where the range of motion of the shoulder and the individual muscles around the shoulder are tested, other tests that are usually required include:
- X-ray of the shoulder – this will show the bones of the joint, and help identify loss of joint space, bone spurs and deformity of the joint.
- CT scan or MRI scan – these scans allow three-dimensional assessment of the shoulder joint and cartilage, and the surrounding muscles and tendons. It also allows for a detailed assessment of the shape and position of the shoulder bones, which becomes essential if planning for surgery.
- Blood tests and joint fluid analysis – sometimes blood tests and a sample of the joint fluid may be required to confirm the cause of arthritis in a joint.
How is shoulder arthritis treated?
Most patients will be candidates for a prescribed course of physiotherapy for several months in order to strengthen the shoulder muscles, maintain range of motion, and improve function.
Anti-inflammatory medication and paracetamol are prescribed for pain relief.
Ultrasound guided injections performed by a radiologist can also be trialled. This should not be performed more than a few times a year.
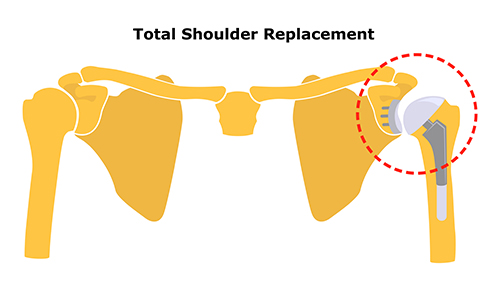
If these non-operative treatments do not improve function adequately, or if there is ongoing pain that is interfering with quality of life, then surgery may be an option. In advanced arthritis, the recommended operation is usually a total shoulder replacement.
My goals as a surgeon are to relieve your pain, restore your function, and return you back to doing what you love.
– Dr Raymond Yu
- Adelaide Orthopaedic Surgeon
- Adelaide Shoulder Surgeon
About
Dr Raymond Yu
Dr Raymond Yu is an Adelaide Orthopaedic Surgeon with post-Fellowship expertise in Shoulder and Elbow Surgery.
He specialises in orthopaedic surgery of the Shoulder and Upper Limb with a focus on modern keyhole and minimally-invasive techniques.
Dr Yu has a special passion for:
- Rotator cuff repair surgery
- Shoulder replacement surgery
- Shoulder stabilisation surgery
Dr Yu practices at